W. K. Lis
Superstar
Doug must be taking advantage of the "exceptions" he's allowed to take, which is why he seems to be missing in action. Then he gets upset with teacher's summer vacation or if someone dares take more than 10 days vacation.
From link.
From link.
The (Ontario) House may meet pursuant to the Standing Orders from Monday to Thursday, from February 16, 2021, to December 9, 2021, with the following exceptions:
March 15 to 18
April 5 to 8
May 24 to 27
June 4 to September 10
September 20
October 11 to 14
November 8 to 11
From link.Canadian Workers Get Fewer Paid Vacation Days Than Nearly Any Other Country in the Industrialized World
Didn’t get much time off work over the holidays? You’re not alone.
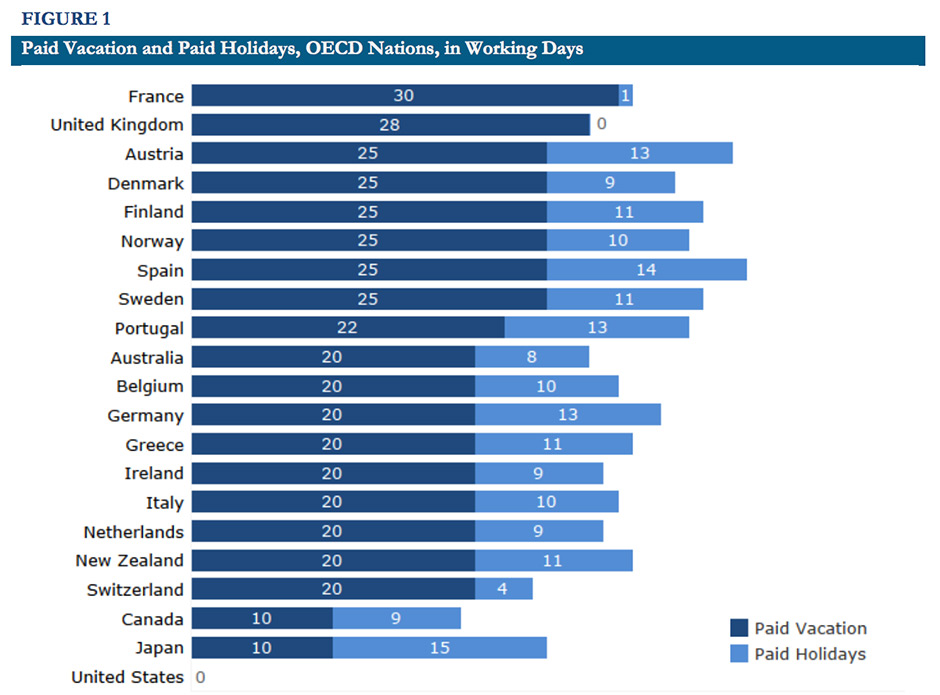
According to a recent study by the Centre For Economic and Policy Research looking into paid vacation and holiday time in countries across the industrialized world, Canada currently ranks near the bottom of the list.
The average Canadian worker only receives 10 paid vacation days each year, tying Canada for second last out of 21 OECD countries in North America, Europe and Asia.
By law, workers in most provinces are only allowed to take up to 10 vacation days off during their first several years of employment with the same employer. However, in Saskatchewan, new workers get three weeks paid vacation.
French workers, by contrast, lead the world with 30 paid vacation days, followed by 28 vacation days enjoyed by British workers.
While Canadian workers also receive nine paid holidays, the 19 days of combined vacation and holidays still places Canada far behind countries like Spain (39 days), Germany (33 days), Sweden (36 days), Norway (35 days) or New Zealand (31 days).
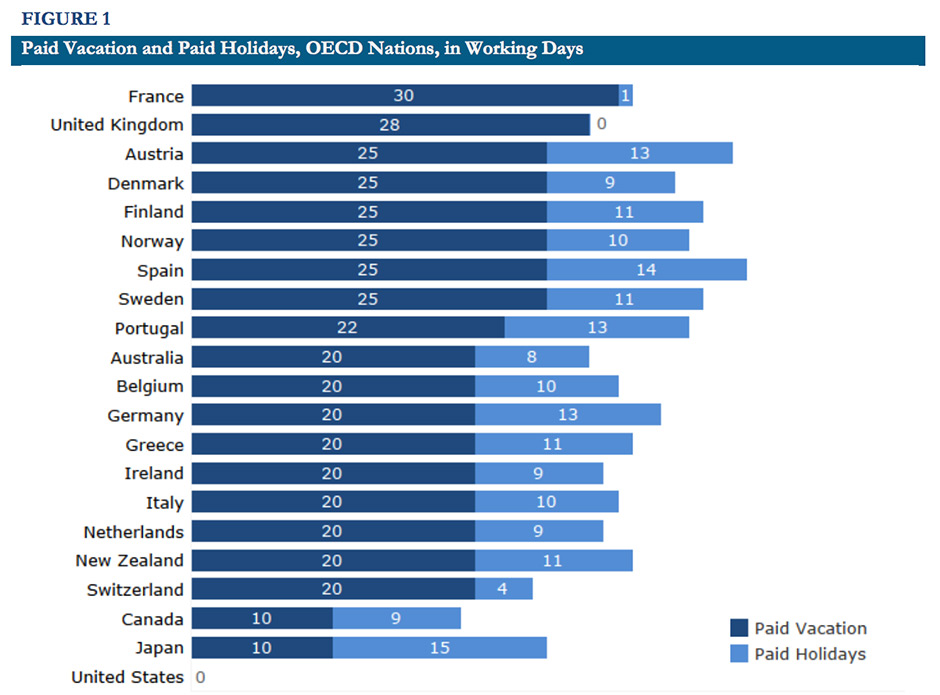
The only country that offers fewer days off to workers is the United States where workers are not entitled by law to paid vacation or holidays.
Japan, which is tied with Canada, has recently launched reforms aimed at reforming the country’s work culture to curb high stress-levels and an epidemic of work-related health problems and suicides.
However, in practice, inequalities within the labour force mean not all workers enjoy the same paid vacation and holidays benefits as the average worker.
“Low-wage, part-time, and small business employees are all far less likely to receive paid vacations or paid holidays,” the study notes.
“When they do receive paid time off, the amount they receive is far less than what is available to their higher-wage, full-time counterparts working for larger employers.”
Greater work-life balance doesn’t just make for happier workers, numerous studies have found numerous social and economic benefits thanks to a healthier and more productive workforce.
In fact, the benefits are so rock-solid, some countries are already going further — Finland, which gives workers 25 paid vacation days, is currently planning to abolish the five-day work week and introduce the three-day weekend.
An experiment by Microsoft in August 2019 found productivity skyrocketed 40% when its Japanese division introduced a four-day work week.
Last edited:







